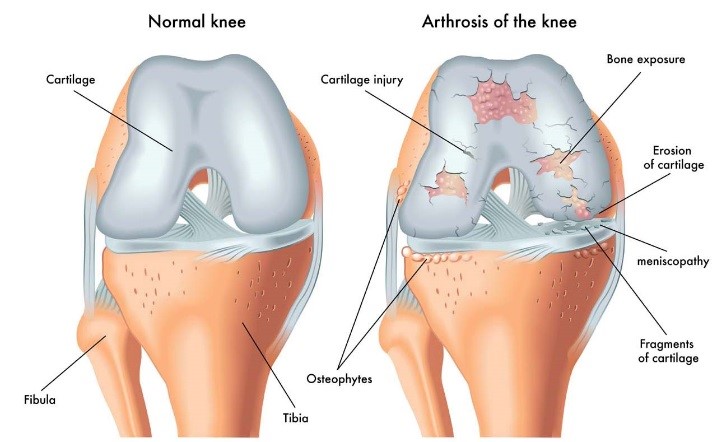
The most common cause of chronic knee pain and disability in the elderly is arthritis. While there are many types of arthritis, most knee pain is caused by just three types – osteoarthritis, rheumatoid arthritis and post-traumatic arthritis.
Osteoarthritis
Osteoarthritis is still the commonest among these three. Osteoarthritis is an age-related "wear and tear" type of arthritis that usually occurs in people 50 years of age and older, but may also occur in younger people. The cartilage that cushions the bones of the knee softens and wears off. The bones then rub against one another, causing knee pain and stiffness.
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability.
Nonsurgical treatment
The initial treatment of arthritis of the knee is usually nonsurgical. Options include:
Lifestyle modifications: Aims to protect your knee joint and slow the progress of arthritis. This involves minimising activities that aggravate the condition such as climbing stairs and squatting or switching from high-impact activities e.g. jogging or badminton, to low-impact activities like swimming or cycling. Losing weight or carrying less heavy objects can also reduce stress on the knee joint.
Physical therapy: Increases the range of motion and flexibility and strengthens the muscles in your thigh to provide more support for the painful knee.
Assistive devices: Using devices such as a cane or crutches to offload the knee.
Topical application: Applying ice to the swelling or heat for comfort, using pain-relieving ointments or creams, or wearing elastic bandages to provide support to the knee may provide some pain relief.
Medication
Several types of drugs are useful in treating arthritis of the knee. These include Acetaminophen or paracetamol (simple, over-the-counter pain relievers that can be effective in reducing arthritis pain) and nonsteroidal anti-inflammatory drugs (NSAIDs), which include ibuprofen and naproxen.
COX-2 inhibitor
This is a special type of NSAID that may cause fewer gastrointestinal side effects. A COX-2 inhibitor reduces inflammation and pain. This medication shouldn’t be used together with NSAIDs if you have had a heart attack, stroke, angina, blood clot, hypertension, or if you are sensitive to aspirin, sulfa drugs or other NSAIDs.
Corticosteroids
Corticosteroids are powerful anti-inflammatory agents that are injected into the joint to reduce inflammation. The effects, however, do not last indefinitely. There is also a need to limit the number of injections to three or four per year and per joint due to possible side effects such as infections or an increase in joint damage.
Viscosupplementation
This involves injecting hyaluronic acid substances into the joint to improve the quality of the joint fluid. Other alternatives include Plate Rich Plasma (PRP).
Glucosamine and chondroitin sulfate
These substances, found naturally in joint cartilage, can be taken as dietary supplements. Although patient reports indicate that they may relieve pain, there is no evidence to support the use of these to decrease or reverse the progression of arthritis.
Others therapies
Many alternative forms of therapy are unproven, but may be helpful provided you find a qualified practitioner and keep your doctor informed. Alternative therapies include the use of acupuncture, soy and avocado extract medication.
Surgical Treatment
Surgical treatment is indicated for:
- Knees that have become bowed and painful as a result of severe arthritis.
- Severe knee pain or stiffness that limits everyday activities, including walking and getting in and out of chairs. You may find it hard to walk more than a few blocks without significant pain, and may need a cane or walker.
- Moderate or severe knee pain while resting, either day or night.
- Chronic knee inflammation and swelling that does not improve with other treatments such as anti-inflammatory medications, cortisone injections, lubricating injections, physical therapy, or other surgeries.
Arthroscopy
Arthroscopic surgery is not often used to treat arthritis of the knee. In cases where osteoarthritis is accompanied by a degenerative meniscal tear, arthroscopic surgery may be recommended to treat the torn meniscus or removing the loose body.
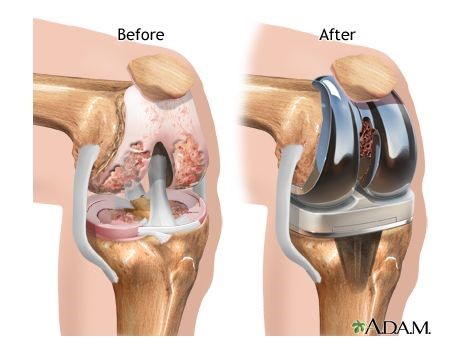
Total or partial knee replacement (arthroplasty)
This removes the damaged cartilage and bone and then positions new metal or plastic joint surfaces to restore knee function. A knee replacement (also called knee arthroplasty) might be more accurately termed a knee "resurfacing" because only the surface of the bones are actually replaced.

There are no absolute age or weight restrictions for total knee replacement surgery.
Recommendations are based on a patient’s pain and disability, not age. Most who undergo total knee replacement are 50 to 80 years of age, but orthopaedic surgeons evaluate patients individually.
An important factor is understanding what the procedure can and cannot, do. More than 90% of people who have total knee replacement surgery experience a dramatic reduction of knee pain and a significant improvement in performing common activities. But total knee replacement will not allow you to do more than you could before you developed arthritis.
With normal use and activity, every knee replacement implant begins to wear in its plastic spacer. Excessive activity or weight may speed up this normal wear and cause the knee replacement to loosen and become painful. Therefore, most surgeons advise against high-impact activities such as running, jogging, jumping, or other high-impact sports for the rest of your life after surgery.
Realistic activities following total knee replacement include unlimited walking, swimming, golf, driving, light hiking, biking, ballroom dancing, and other low-impact sports.
With appropriate activity modification, knee replacements can last for many years.
Possible surgical complications
The complication rate following total knee replacement is low. Serious complications such as knee joint infections occur in fewer than 2% of patients. Major medical complications such as heart attacks or strokes occur even less frequently. Chronic illnesses may increase the potential for complications. Although uncommon, when these complications occur, they can prolong or limit full recovery.
Infection
Infection may occur in the wound or deep around the prosthesis. It may happen while in the hospital, after you go home or even years later. Minor infections in the wound area are generally treated with antibiotics. Major or deep infections may require more surgery and removal of the prosthesis. Any infection in your body can spread to your joint replacement.
Blood clots
Blood clots in the leg veins are one of the most common complications of knee replacement surgery. These clots can be life-threatening if they break free and travel to your lungs. Your orthopaedic surgeon will outline a prevention programme, which may include periodic elevation of your legs, lower leg exercises to increase circulation, support stockings and blood-thinning medication.
Implant problems
Although implant designs, materials and surgical techniques continue to advance, implant surfaces may wear down and components may loosen. Additionally, although an average of 115° of motion is generally anticipated after surgery, scarring of the knee can occasionally occur and motion may be more limited particularly in patients with limited motion before surgery.
Continued pain
A small number of patients continue to have pain after a knee replacement. This complication is rare, however, and the vast majority of patients experience excellent pain relief following knee replacement.
Neurovascular injury
While rare, injury to the nerves or blood vessels around the knee can occur during surgery.
Anesthesia
The most common types of anesthesia are general anesthesia (you are put to sleep) or spinal, epidural anesthesia (you are awake but your body is numb from the waist down). With your input, the anesthesia team will determine which type of anesthesia is best for you.
Procedure
The procedure itself takes approximately 1 to 2 hours. An orthopaedic surgeon will remove the damaged cartilage and bone, and then position the new metal and plastic implants to restore the alignment and function of your knee.
Different types of knee implants are used to meet each patient’s individual needs.
After surgery, you will be moved to the recovery room, where you will remain for 1-2 hours while your recovery from anesthesia is monitored. After you wake up, you will be moved to your hospital’s high dependency unit (HDU).Subsequent stays will range from 3-5 days with daily physiotherapy
How your new knee is different
Improving knee motion is a goal of total knee replacement, but restoration of full motion is uncommon. Knee replacement motion after surgery can be predicted by the range of motion you have in your knee pre-surgery. Most patients can expect to almost fully straighten the replaced knee, bend it sufficiently to climb stairs and get in and out of a car. Kneeling is sometimes uncomfortable, and although not harmful should be avoided if possible.
Most people feel some numbness in the skin around the incision and outer aspect of the knee. There may also be some stiffness, particularly with excessive bending activities.
Most people also feel or hear some clicking of the metal and plastic with knee bending or walking. This is normal. These differences often diminish with time, with most patients finding them tolerable when compared with the pain and limited function they experience prior to surgery.
Your new knee may activate metal detectors in airports and other buildings. Inform security about your knee replacement if an alarm is activated.
Protecting your knee replacement
After surgery, make sure you also do the following:
- Participate in regular, light exercises to maintain proper strength and mobility.
- Take special precautions to avoid falls and injuries. If you break a leg bone, you may require more surgery.
- Ensure your dentist knows about your knee replacement. Talk with your orthopaedic surgeon about whether you need to take antibiotics prior to dental procedures.
- See your orthopaedic surgeon periodically for follow-up examinations and X-rays.
Extending the life of your knee implant
Currently, more than 90% of modern total knee replacements still function well 15 years after surgery. Keep in mind that following your orthopaedic surgeon’s instructions post-surgery and caring for your knee replacement and general health allows you to contribute to the final success of your surgery.