Knee replacement surgery is usually recommended for people with severe osteoarthritis when other treatment modules such as medications, exercise or pain-relief methods are no longer working. Surgery helps relieve the pain that keeps patients from their daily activities such as walking, driving or getting out of bed.
With medical advancements, many knee surgeries are less invasive, faster and safer than before. However, proper after-care after surgery is important for prompt recovery. If you or your loved one will be undergoing knee surgery, here is what you need to know to prepare ahead:
DURING SURGERY
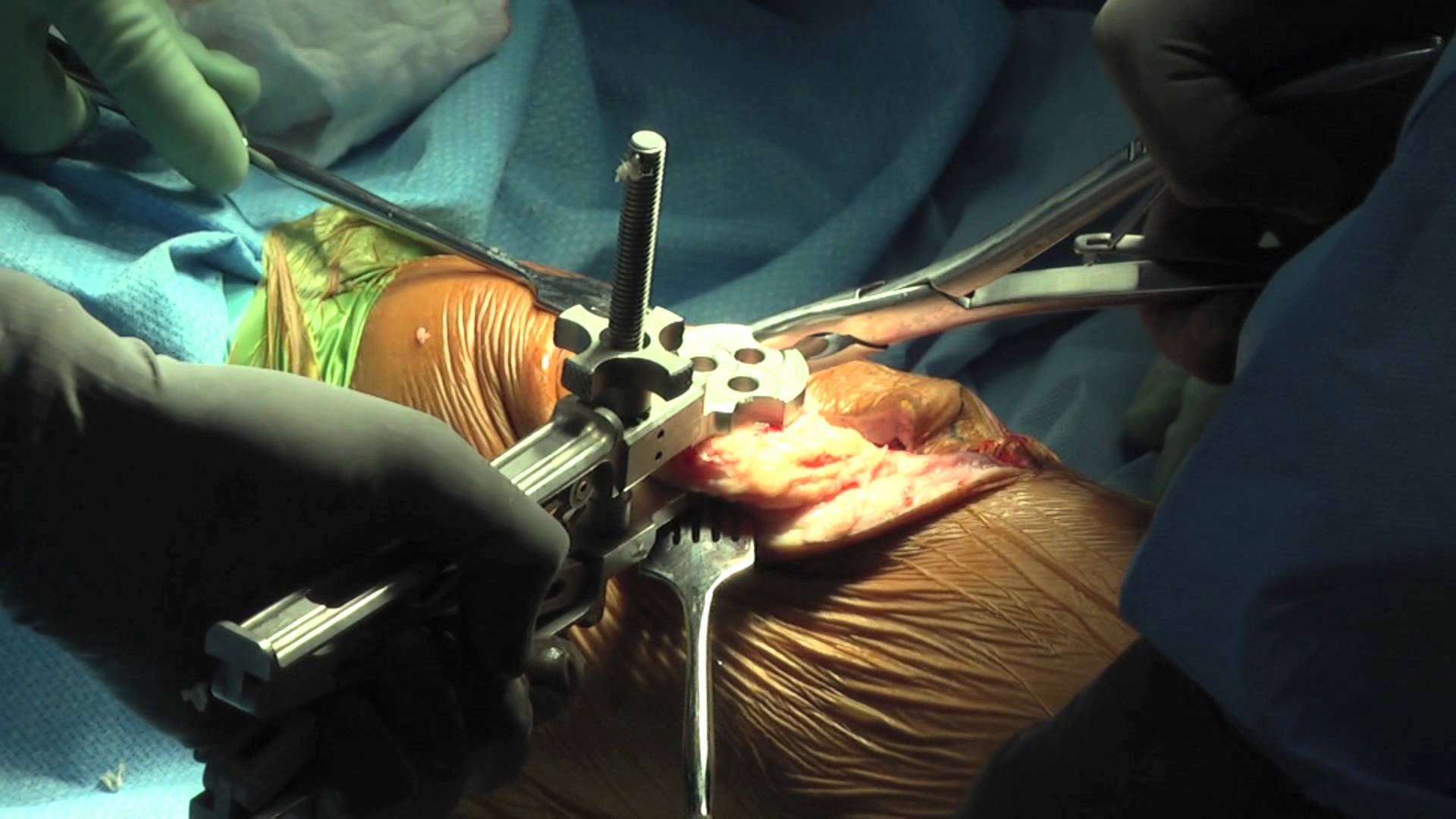
You will be put under general anaesthesia or regional anaesthesia (spinal or combined spiral) and will be unconscious during the surgery. The surgeon will make a cut at the knee, remove the damaged cartilage and replace it with an artificial joint. Although the surgery itself takes only 1-2 hours, the entire process will take up to 5-6 hours, including preparation time pre-surgery, anaesthetic administration and post-surgical procedures.
AFTER SURGERY

When you wake up after surgery, you will find an intravenous (IV) tube hooked to your arm to administer pain medications and even a urinary catheter to help you pass urine.
Despite that, you will be encouraged to get out of bed the next day or as soon as tolerated and start walking around to promote blood circulation and speed up recovery. For better support, you can use parallel bars or other walking devices such as walker frames to walk around.
Your knee will appear swollen, bruised and sore for a few days after surgery. You will be ready for discharge after 4-5 days in hospital.
AFTER DISCHARGE

Caring for yourself becomes more important after you go home. Most patients report improvements in their condition after a few days of rest, but knowing what to expect will help in the recovery process. Here is what you need to know so that you can better prepare yourself:
MEDICATIONS AND PAIN RELIEF – Remember to take your medications as instructed by your doctor as they will help with pain relief and infection prevention. If your wound hurts badly, contact your doctor to check if stronger medications are required. Within the second or third week, you will begin to feel better.
SUPPORT SYSTEM – It is necessary to have someone around the first week or so after your surgery to help with daily activities such as cooking, cleaning or taking care of other matters so that you can focus on your recovery. You may also feel tired, in pain and frustrated at your loss of independence, so having a loved one to help you move around, stay comfortable and drive you to follow-ups, is essential for speedy recovery.
DEPRESSION – One often overlooked aspect post surgery is the state of mind. You may feel anxious, scared, tired, in pain and helpless as you temporarily depend on others to help you with eating, bathing, changing and other responsibilities. Left unaddressed, it could sometimes lead to depression. Share your feelings with someone and seek advice from your doctor, who will be able to provide solutions. The depressive mood will usually lift once you recover and start resuming your normal activities.
BATHING – Many patients are anxious about taking baths after surgery but it is alright to take a warm shower as long as the wound site is kept dry with a plastic wrap. You may need someone to help you undress and dress in the first few days. Bring a plastic chair into the bathroom to sit on as you shower in case you lose your balance. You will be surprised how much better you will feel after a warm, refreshing shower!
INSOMNIA – Some patients report inability to sleep after surgery due to soreness, fatigue or anxiety. Try practising relaxation methods such as drinking chamomile tea, listening to relaxing music, using aromatherapy and avoiding caffeinated food and drinks from evening onwards. If nothing works, speak to your doctor on whether you can have sleeping pills for a short period to help you get the much-needed rest, pain control also important to make you comfortable and able to go to sleep.
NUTRITION – After surgery, avoid foods that are high in Vitamin K such as broccoli, cauliflower, Brussels sprouts, liver, green beans, lentils, soybeans, kailan, cabbage, and onions as they may contribute to blood clotting. Even if your appetite is poor, you must continue to take a healthy diet so that your body can recover. Apart from having a balanced diet according to the food pyramid, you might want to supplement with Vitamins C and D, or supplements such as coenzyme Q10, essential fatty acids, free-form amino acids, L-lysine, L-cysteine, L-glutamine or MSM to aid cell renewal. Check with your doctor before beginning any nutritional supplements.
WOUND CARE – Observe your wound daily to see if there are any unexpected changes such as swelling, pain or infection. See the doctor for scheduled follow-ups for dressing changes and inform him if you notice anything abnormal.
BRUISING AND SWELLING – After surgery, the body will send heavy blood flow to the area as a recovery mechanism. This creates the wound area to have a ‘blue black’ and swollen effect. To reduce the swelling and bruising on your operated knee, elevate your leg by lying down and placing your leg on a pillow, higher than your head, for an hour or two every afternoon or evening.
COMPRESSION STOCKINGS – Your doctor may recommend that you wear compression stockings to sleep for the first month. These long stockings firmly grip your leg, helping to reduce soreness and the risk of developing a blood clot (Deep Vein Thrombosis)
REHABILITATION AND PHYSIOTHERAPY – Rehab is an important element of any surgery to prevent muscle wastage, build strength and promote healing. The therapist at the hospital will teach you how to conduct low-impact exercises and encourage you to continue performing them regularly at home for maximum impact. In some cases, the therapist may recommend using Transcutaneous Electrical Nerve Stimulation (TENS) to stimulate blood flow and reduce pain at the surgical area. This is where some electrically charged pads will be placed at your leg and turned on while you relax for 15-20 minutes.

RESUMING DAILY ACTIVITIES – Most patients will be able to resume light activities such as walking and standing within 2 weeks. More strenuous activities such as driving, sexual activities and exercise can be resumed within 6 weeks. Choose low-impact exercise such as swimming, walking or taichi and avoid jerky or jumping movements.
ORGANISING MEDICAL CARE – Keep a folder for all your medical bills as they may come from different departments each time you visit the hospital. Place the contact details of your doctor or hospital in a conspicuous place so that your caregivers can help call them on your behalf if necessary. Keep track of your hospital appointments carefully so that you do not miss your follow-up sessions to monitor your healing progress.
HOME IMPROVEMENTS – Families with ageing parents may want to consider minor renovations that will greatly assist improve safety and comfort levels of elderly people. These include fixing grip bars along the walls and in the bathroom, having non-slip floor mats, removing carpets that might cause tripping, fixing night lights in common areas such as the kitchen, bathroom and living room, and having a shower seat installed.