With the increase in the aging population, the study and care of gastrointestinal disorders in the elderly have become priority topics for clinicians and researchers, who aim to create more awareness on the effects of aging upon the physiology of the gastrointestinal (GI) tract.
Although an increased prevalence of several common gastrointestinal disorders occurs in the elderly person, aging per se appears to have less direct effect on most gastrointestinal functions, in large part due to the functional reserve of the gastrointestinal tract. As the digestive system has a lot of reserves built into it, aging has less effect on its function than it does on the function of other organ systems. Nonetheless, aging is a factor in several digestive system disorders.
From a chronological viewpoint, medical treatment of the elderly (geriatrics) starts from the age of 65. This definition is nowadays certainly not really an adequate definition of an elderly patient and the reason to be treated by a geriatrician.
Gastrointestinal diseases refer to diseases involving the GI tract, namely the esophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.
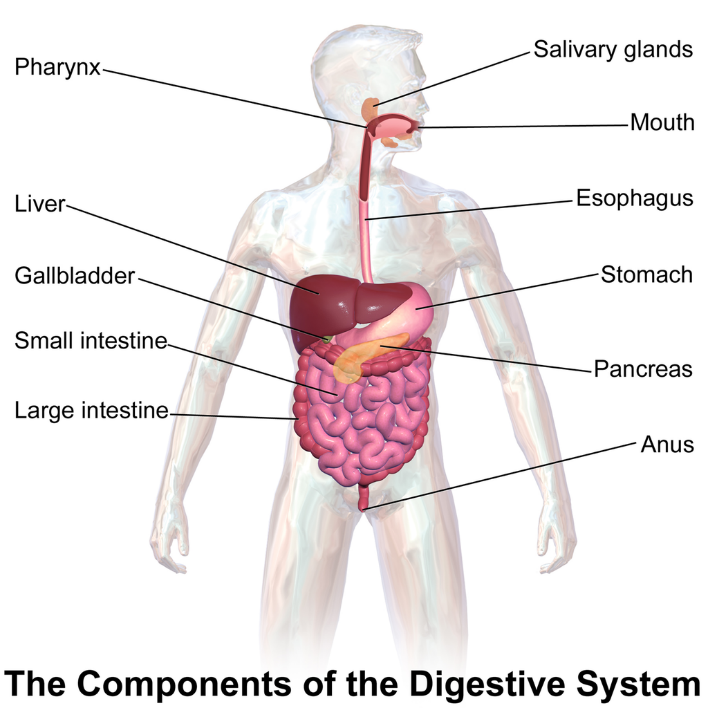
(Source: https://en.wikipedia.org/wiki/Gastrointestinal_disease)
A gastroenterologist frequently encounters elderly patients with complaints of GI diseases. Understanding age-related changes in gastrointestinal physiology and the effects of common co-morbid illnesses enhances the ability to evaluate and treat these common, troublesome symptoms.
Here’s an overview of common digestive health problems that may arise with age. Learn why they occur and what you can do to keep your system running smoothly well into your later years.
Digestive problems common to the elderly
- Oral health. Poor oral health can contribute to various GI symptoms. For example, dental decay and changes in dentition can disrupt nutritional status and cause constipation. Tooth loss is associated with age-related decline in bone mass and calcium content in the skeleton. Soft, easy-to-process foods are preferable for the edentulous, but they often lack fibre, which can impact colonic transit as many fibres have a laxative effect.
- Changes in the digestive system & constipation. The digestive system moves food through the body by a series of muscle contractions. As one ages, this process sometimes slows down and causes food to move more slowly through the colon. When things slow down, more water gets absorbed from food waste, which can cause constipation. Symptoms include difficult or painful bowel movements, infrequent bowel movements, and hard, dry stool.
There are a number of age-related factors that can cause constipation in older adults like drinking insufficient fluids. Staying hydrated helps prevent constipation at any age. It can become more of an issue for older adults who take diuretics for high blood pressure or heart failure. Diuretics lower blood pressure by causing you to lose excess fluid by urinating more often. Some people may avoid drinking too many fluids so they don’t have to run to the bathroom all day long. Between urinating more and drinking less, you can become dehydrated.
- Medication use. Several common medications can cause constipation. One example is calcium channel blockers, used for high blood pressure. Narcotic pain relievers are another common culprit.
- Inactivity. People often become less active as they age. Bed rest during an illness can cause real problems.
- Diverticular disease. About half of people age 60 and older have diverticulosis. This occurs when small pouches in the lining of the colon bulge out along weak spots in the intestinal wall. While many people don’t have any symptoms, gas, bloating, cramps, and constipation may occur. While they don’t usually cause a problem and require treatment, they can cause scarring and irregularity. If the pockets become inflamed, it’s called diverticulitis, which can cause abdominal pain, cramping, fever, chills, nausea, and vomiting. Antibiotics, pain medications, and a liquid diet can treat diverticulitis.
- Ulcers & NSAIDs. Many older adults use nonsteroidal anti-inflammatory drugs (NSAIDs) to control pain from arthritis and other types of chronic pain. Regular use of NSAIDs increases the risk for stomach bleeding and ulcers. While aging alone doesn’t make the stomach more prone to ulcers, the chronic use of NSAIDs does raise the risk.
- Problems with the mouth and esophagus. The esophagus is the tube that connects the mouth to the stomach. Like the colon, the esophagus can also slow down with age, moving food through more slowly. This can cause problems swallowing food or fluids. Dementia, stroke, and conditions such as Parkinson’s disease can also cause difficulty in swallowing.
- Polyps. After the age of 50, the risk increases for developing polyps (small growths) in the colon. Polyps may be noncancerous, they may become cancer, or they may be cancer. Screening colonoscopies are recommended for anyone over the age of 50 as during this procedure, polyps can be removed before they become cancer. People with a family history of colon cancer or other risk factors may need screenings earlier.
- GERD. Gastroesophageal reflux disease (GERD) is the most common upper GI disorder in older adults, although people of all ages can get it. GERD occurs when stomach acid backs up into the esophagus, causing heartburn and other symptoms. Eating late at night and eating the wrong types of foods, such as fast food and fried foods, can all cause reflux. Certain medications, including some blood pressure medications can also cause heartburn. Obesity increases your risk for heartburn and GERD.
- Pelvic floor disorders. Anorectal dyssynergy or paradoxical anal contractions can lead to incomplete emptying of the rectum. Diabetes can further contribute to constipation due to delayed transit times secondary to autonomic neuropathy. Age-related changes in the physical structure and function of the pelvic floor likely contribute to constipation and fecal incontinence.
- Diarrhea. This can result from food-borne illness, antibiotic use, fecal impaction, colon cancer, carbohydrate malabsorption, SIBO (small intestinal bacterial overgrowth) or overproduction of bile acid.
- Lactose Intolerance. Lactose intolerance increases with advanced age, with one study showing it to occur in 50% of elderly subjects. Of those with lactose intolerance, 90% were present with SIBO.
- Fecal incontinence. This may occur due to pelvic floor dysfunction, which may develop due to obstetrical injury or with decreased rectal compliance that can accompany aging. Fecal incontinence is common in middle age and also may occur due to chronic constipation, diarrhea or chronic diseases such as multiple sclerosis or diabetes.
- Hormone changes. In women, GI (gastrointestinal) symptoms are often exacerbated during menses and early menopause, suggesting that a decline in the ovarian hormones estrogen and progesterone may play a role. As women age, their abdominal muscles weaken, and there’s more abdominal bulge after eating. Abdominal bloating is also a symptom of ovarian cancer, so if the symptoms don’t improve by eating smaller meals and increasing exercise, then further investigation by a gynecologist or primary care physician should be initiated.
Help for digestive problems associated with aging
Diet can help manage GI symptoms associated with aging. Reducing meal size and intake of high-fat foods and modifying caffeine and alcohol consumption can reduce GERD symptoms. Weight and stress management are other ways to address GI symptoms related to GERD.
- Eat a low-fat, high-fiber diet, rich in fruits and vegetables. Substitute brown for white.
- Stay hydrated by drinking adequate water.
- Exercise e.g. walking, bike riding, gardening or swimming.
- Practice moderation when indulging in coffee, wine, chocolate and other occasional extravagances.
- Know the warning signs of serious digestive problems – progressive abdominal pain, sudden weight loss and unexplained bleeding always deserve an evaluation.
- Eat gut-friendly foods. The healthy bacteria levels in your gut can be further boosted by increasing dietary prebiotics (oats, bananas, leeks, onions, garlic), polyphenols (blueberries, cocoa, green tea) and fermented foods (kefir, kombucha, kimchi, sauerkraut, miso). By eating an array of these foods (the more diverse the better) and minimising sugary foods, you can help to encourage the growth of beneficial bacteria and provide a good environment for the healthy digestion and absorption of nutrients.
- Consider a probiotic. The "live" bacteria in our digestive tract are known to have a huge impact on digestive health, and research has shown that bacteria composition changes with age. Low levels of bacteria may manifest as symptoms such as constipation and bloating. A way to enhance their population is to supplement with a good quality probiotic supplement.
- Support stomach acid. In older individuals, conditions that decrease stomach acid secretion such as gastritis become more common. Certain medications (such as PPIs) and chronic stress can also impact on this. Individuals can support stomach acid production through a number of dietary interventions including relaxing and eating slowly at mealtimes and drinking room-temperature or warm water or tea with meals rather than chilled drinks.
- Speak to your doctor about medication. One of the major contributors to digestive distress in older adults is prescription medicine. Pay attention to your medication by asking a doctor or pharmacist what impact it may have on your digestive system. Don’t take additional medication unless there is a clear, current need, and evaluate your medication list with your doctor on a regular basis.
Last but not the least, if you are concerned about GI diseases and their symptoms, do consult your doctor.